The International Society of Sports Nutrition published in 2017 a position stand (see reference below) on the safety and efficacy of creatine supplementation in the context of exercise, sports and medicine.
Creatine supplementation, one of the most popular and studied nutritional supplements, has in fact been shown to be effective in improving athletic performance (especially in high intensity exercise) and inducing relevant training adaptations. The consequent increase in intramuscular creatine (and phosphocreatine) reserves facilitates the rapid re-synthesis of ATP, the so-called energy “currency” of the body, which is essential for almost every reaction in our body. Thus, the increased availability of creatine in the cell through supplementation contributes to improve performance because it increases the energy availability in order to exercise (i.e. muscle contraction) as well as a whole range of other muscle cell related reactions. Creatine supplementation can in fact enhance strength production, muscle work, accelerate recovery and help preventing injury.
Additionally, creatine supplementation appears to be highly safe and effective not only in athletes but also in non-athletes (such as the so-called exercise enthusiasts), as well as in various clinical populations. In fact, several studies (see ISSN article, reference below) point to benefits of creatine supplementation in various populations and clinical settings, such as:
– Accelerating injury rehabilitation (because it attenuates muscle atrophy);
– Protection of neuronal injuries (spinal and cerebral);
– Mitigation of debilitating consequences in people with congenital syndromes of creatine synthesis deficiency;
– Attenuating the progression of neurodegenerative diseases (e.g. Huntington’s disease, disease, Parkinson’s disease, mitochondrial diseases, amyotrophic lateral sclerosis);
– Prevention and / or improvement of bioenergetics in patients with myocardial ischemia or stroke victims;
– Improving metabolic and functional indicators associated with aging;
– Possible benefit during pregnancy for optimal growth, development and health of the fetus.
In conclusion, creatine does indeed appear to be a safe and beneficial nutritional supplement for a wide range of populations and ages. Indeed, this is a supplement that actually works!
Take creatine and power to you!
Nuno Correia
References:
Kreider, R.B. et al., 2017. International Society of Sports Nutrition position stand: safety and efficacy of creatine supplementation in exercise, sport, and medicine. Journal of the International Society of Sports Nutrition, 14(1), p.18. Available at: http://jissn.biomedcentral.com/articles/10.1186/s12970-017-0173-z.
In order to maintain physical function, recover better from injury, maintain lean mass and stay healthier overall, older individuals need a higher protein intake than younger individuals. Higher protein intake contributes for attenuating inflammatory and catabolic processes, as well as ameliorating the decreased efficiency in protein metabolism associated with age.
According to the recommendations advanced by the PROT-AGE Study Group (2013) (reference below), older individuals should:
– eat at least 1 to 1.2g/kg body weight of protein per day;
– eat MORE protein if suffering from acute or chronic illness, between 1.2-1.5g/kg body weight of protein per day;
– ingest EVEN MORE if malnourished and / or suffering from severe illness or injury, ~2g/kg body weight of protein per day;
– limit protein intake if suffering from SEVERE KIDNEY DISEASE and NOT following hemodialysis. These individuals are therefore an EXCEPTION concerning protein intake;
– use supplementation to the achieve desired protein intake levels;
– and, of course, DO the type of exercise that most effectively promotes the maintenance or increases in lean mass, which is strength training.
And no, kidney disease is NOT caused by protein intake. In a one-year follow-up study with resistance-trained men consuming ~2.51-3.32 g/kg of body weight per day for one year, there were no harmful effects on measures of blood lipids as well as liver and kidney function (Antonio et al, 2016).
Maintaining strength and lean mass (including muscle mass, bone and connective tissue mass) are identified as the first and most relevant biomarkers of health and longevity. Improving these markers produces a positive and powerful “domino effect” on most (probably all) of the other health markers. Proper protein intake and strength training is essential for building lean mass. And even more crucial as we age in order to counteract the inevitable progressive loss of efficiency in our metabolism.
Do not fear protein nor strength training. These are probably two of your best allies to live better and longer.
Don’t forget the protein at your next meal!
Nuno Correia
References:
Bauer, J. et al., 2013. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the prot-age study group. Journal of the American Medical Directors Association, 14(8), pp.542–559.
Antonio, J., Ellerbroek, A., Silver, T., Vargas, L., Tamayo, A., Buehn, R., & Peacock, C. A. (2016). A High Protein Diet Has No Harmful Effects: A One-Year Crossover Study in Resistance-Trained Males. Journal of nutrition and metabolism, 2016, 9104792.
“People don’t decide their future, people decide their habits and their habits decide their future.”
– F.M. Alexander
Nine years ago (2010)1, the European Working Group on Sarcopenia in Older People (EWGSOP) published a definition of sarcopenia that has been widely used worldwide and this definition has fostered advances in the identification and care of people at risk or with sarcopenia. It was defined as a syndrome characterized by progressive and widespread loss of muscle mass and strength at risk of adverse outcomes such as physical disability, poor quality of life and death. Because the relationship between muscle mass and strength is not linear (the ability to generate strength is not only dependent of muscle mass), the criteria for its diagnosis included low muscle mass and low muscle function (i.e. strength or physical performance).
After learning that in 2016 sarcopenia was classified as a disease by the World Health Organization, as noted in the first part of this article, the EWGSOP22 updated its operational definition and various diagnostic strategies, considering now that muscle strength (measured by grip strength or the chair stand test) is the main parameter for measuring muscle function, even more important than the amount of muscle mass. Therefore, it is in this context that we justify the title of this article and reinforce the importance of sharing this message with all health professionals.
The implications of this condition on human health are several and widely known: increased risk of falls and fractures3,4; impairment of activities of daily living5; association with heart disease6; respiratory disease7 and cognitive dysfunction8; lower quality of life9; loss of independence10,11,12 and death13. In financial terms, public health costs have also been calculated in several papers. In a study by Janssen et. al.14, in 2004, the costs of sarcopenia in the United States were estimated at $ 18.5 billion annually, representing about 1.5% of total health costs. In a study conducted here in Portugal at the Hospital de Santo António in Porto and published in 201615, it was found that hospitalization costs associated with sarcopenia were higher by 58.5% for patients under 65 years and by 34% for patients aged 65 and over. More recently (2018), the Hertfordshire Cohort Study in the United Kingdom16 found that the costs associated with lack of muscle strength were estimated at £ 2.5 billion annually.
In the present scenario, where the phenotype of unhealthy aging is proliferating in the eyes of all industrialized nations, in which diseases such as hypertension, cancer, depression, Alzheimer’s disease and type II diabetes are destroying people’s lives, it is essential to adopt measures aimed at improving function of each individual rather than diagnosing illnesses and administering medicines which, in addition, do not help solving this problem, and may further aggravate their condition. We know that the main health problems are related to poor diet, physical inactivity, lack of sleep, excess alcohol, exposure to tobacco and polluted environments but also lack of movement quality, vigor and muscular strength.
The benefits of strength training in health are well supported in the scientific literature and the most important ones are: decrease in blood pressure; decreased risk of osteoporosis and sarcopenia; improvement of lipid profile; increased cardiorespiratory capacity; prevention and management of chronic pain; increased insulin sensitivity; improvement of wellbeing and self-confidence. Moreover, several studies17,18,19 have shown a strong and consistent correlation between increased strength and muscle mass with decreased mortality, reinforcing the fact that the decline in strength associated with the current levels of sedentarism and aging need to be addressed. Therefore, a well-designed strength training program that meets the individual’s competency and follows the principles of adaptation to training will improve all of the above health indicators and all the necessary physical qualities (strength, power, speed, agility, balance, coordination, mobility, endurance) to carry out the activities of our daily life. These are the parameters of physical function that are currently being proposed as biomarkers of aging in humans20.
Consequently, program design will be the determining factor in this equation. And while it is true that this process requires imperative knowledge of sports sciences, it must be borne in mind that it also requires field work and art in coaching. Instead of being so preoccupied with following the guidelines and looking for statistically significant results, we should be concerned that our approach is relevant to one’s life. Because we work with people. People who have time constraints to train. People with different family and professional responsibilities. People who have different lives from each other. People who have a host of metabolic and / or orthopedic problems that no randomized controlled trial can ever reproduce! Yes, this is a complex process.
Finally, we know that one of the mechanisms responsible for muscle atrophy, sarcopenia and aging is apoptosis, a form of programmed cell death and a fundamental process in aging. But when we train, eat and rest properly, we are sending a signal to our body to create an anabolic environment, an environment that enhances the release of growth factors and suppresses apoptosis. That is, strength training is a macroscopic growth factor that suppresses programmed cell death (i.e. apoptosis), but unlike drugs, where an increasing in dose means more disease and dependence, an increase in load (even if reduced) means more health, more strength and more vigor. This way, the daily decisions will always be up to each one: treat the body like a Ferrari or treat the body like a rental car.
Pedro Correia
References:
- Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing 2010; 39: 412–23.
- Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M; Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019 Jan 1;48(1):16-31.
- Bischoff-Ferrari HA, Orav JE, Kanis JA et al. Comparative performance of current definitions of sarcopenia against the prospective incidence of falls among community-dwelling seniors age 65 and older. Osteoporos Int 2015; 26:2793–802.
- Schaap LA, van Schoor NM, Lips P et al. Associations of sarcopenia definitions, and their components, with the incidence of recurrent falling and fractures: the longitudinal aging study Amsterdam. J Gerontol A Biol Sci Med Sci 2018; 73: 1199–204.
- Malmstrom TK, Miller DK, Simonsick EM et al. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 2016; 7: 28–36.
- Bahat G, Ilhan B. Sarcopenia and the cardiometabolic syndrome: a narrative review. Eur Geriatr Med 2016; 6: 220–23.
- Bone AE, Hepgul N, Kon S et al. Sarcopenia and frailty in chronic respiratory disease. Chron Respir Dis 2017; 14: 85–99.
- Chang KV, Hsu TH, Wu WT et al. Association between sarcopenia and cognitive impairment: a systematic review and metaanalysis. J Am Med Dir Assoc 2016; 17: 1164.e7–64.e15.
- Beaudart C, Biver E, Reginster JY et al. Validation of the SarQoL(R), a specific health-related quality of life questionnaire for Sarcopenia. J Cachexia Sarcopenia Muscle 2017; 8: 238–44.
- Dos Santos L, Cyrino ES, Antunes M et al. Sarcopenia and physical independence in older adults: the independent and synergic role of muscle mass and muscle function. J Cachexia Sarcopenia Muscle 2017; 8: 245–50.
- Akune T, Muraki S, Oka H et al. Incidence of certified need of care in the long-term care insurance system and its risk factors in the elderly of Japanese population-based cohorts: the ROAD study. Geriatr Gerontol Int 2014; 14: 695–701.
- Steffl M, Bohannon RW, Sontakova L et al. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging 2017; 12: 835–45.
- De Buyser SL, Petrovic M, Taes YE et al. Validation of the FNIH sarcopenia criteria and SOF frailty index as predictors of long-term mortality in ambulatory older men. Age Ageing 2016; 45: 602–8.
- Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004 Jan;52(1):80-5.
- Sousa AS, Guerra RS, Fonseca I, Pichel F, Ferreira S, Amaral TF. Financial impact of sarcopenia on hospitalization costs. Eur J Clin Nutr. 2016 Sep;70(9):1046-51. doi: 10.1038/ejcn.2016.73. Epub 2016 May 11.
- Pinedo Villanueva, R. A., Westbury, L. D., Syddall, H. E., Sanchez, M., Dennison, E. M., Robinson, S. M., & Cooper, C. (2018). Health care costs associated with muscle weakness: a UK population-based estimate. Calcified Tissue International.
- Ruiz JR, Sui X, Lobelo F, et al. Association between muscular strength and mortality in men: prospective cohort study. BMJ. 2008;337(7661):a439. Published. doi:10.1136/bmj.a439.
- Srikanthan P, Karlamangla AS. Muscle mass index as a predictor of longevity in older adults. Am J Med. 2014;127(6):547-53.
- Dos Santos L, Cyrino ES, Antunes M, Santos DA, Sardinha LB. Changes in phase angle and body composition induced by resistance training in older women. Eur J Clin Nutr. 2016 Dec;70(12):1408-1413. doi: 10.1038/ejcn.2016.124. Epub 2016 Jul 13. PubMed PMID: 27406159.
- Cadore EL, Izquierdo M. Muscle Power Training: A Hallmark for Muscle Function Retaining in Frail Clinical Setting. J Am Med Dir Assoc. 2018 Mar;19(3):190-192.
There is currently sufficient scientific evidence to assert that strength training is an effective method for preventing, treating and potentially reversing various chronic diseases. Indeed, adherence to a properly designed strength training program can significantly increase the physical and mental health of the population.
The importance is such that several world-renowned organizations (World Health Organization, Centers for Disease Control and Prevention, American Heart Association, American Association for Cardiovascular and Pulmonary Rehabilitation, American College of Sports Medicine) recommend this form of training for maintain health.
However, despite this evidence, most of exercise recommendations are still for aerobic training, and few physicians (and health professionals in general) recommend strength training. This article aims to alert for the relevance and valuable impact of strength training on health.
About 100% of our biological existence has been dominated by outdoor activity. Hunting and searching for food has been a condition of human life for millions of years1. That is, if in the past it took effort (i.e. physical activity) to find food, nowadays food comes to us without having to make any effort. Therefore, we have moved from a very active lifestyle to a highly sedentary lifestyle. With serious consequences for public health. If in the past all people had to engage in some sort of physical exertion to carry out their daily tasks, today most of them do not have those needs. The environment has changed and so have people. They are weaker, sicker, have more chronic pain and are increasingly dependent on medicines. But the message still going on in our society (and passed on in medical appointments) is “make no physical efforts and follow your normal life”. And I believe this is the worst advice people can get! Normal life? But what kind of advice is this? How can normal be good? You must be completely alienated from reality in order to make such recommendations.
Today we have more opportunities than ever to build a healthy and strong phenotype. The phenotype is the expression of our organism, and it depends largely on the choices we make every day. Two organisms can have the same genotype, the same DNA, but different phenotypes – based on their experiences and the environment. Admittedly, there are things we cannot control such as our genetic heritage, the place of the world where we were born / lived, overall luck and the general environment to some extent. But there are many things that we can control that depend solely on our priorities in life and our daily choices (examples: exercise habits, eating, sleeping, stress management, smoking, alcohol, exposure to polluted environments). And I believe that exercise in general (and strength training in particular) is the most important factor of all. It is the most potent, it’s quantifiable and acts quickly on all systems and organs of the human body.
The reality is this: the population is aging and with more chronic / noncommunicable diseases. The main noncommunicable diseases are cardiovascular diseases, cancers, chronic respiratory diseases and diabetes. These four disease groups alone account for over 80% of the 41 million deaths in the world2! According to the first report on healthy aging by the World Health Organization (WHO), the number of people over 60 is expected to double by 20503, and it is in this context that we need to urgently intervene to promote motor autonomy and improve people’s functional capacity. Traditional recommendations for walking, swimming, Pilates, and “doing low effort activities” or “no physical effort” probably need to be reconsidered and properly contextualized.
It is in this context that strength training and athletic training play a key role. All people (athletes and non-athletes) need to train their physical qualities to live with quality and independently. After age 30, adults lose 3-8% of their muscle mass per decade. Over time, the loss of lean mass contributes to a decrease in muscle strength and power, which are important predictors of balance, falls and mortality4. In the case of the elderly, it is important to note that falls are the main cause of accidental death after age 65 and hip fractures are those that most affect their independence5.
When I speak of strength I mean the basis for interacting with the environment around us, the foundation for the development of other physical qualities (mobility, power, speed, agility, muscle endurance), the ability to produce strength against external resistance (it can be the floor or any other object) through muscle contractions. This is probably the most trainable capacity we have and the one that could have the greatest impact on improving our function, independence and functional longevity. Tasks such as brisk walking, sitting and rising from a chair, climbing stairs, maintaining balance, carrying luggage, or playing with children / grandchildren are examples of activities in our daily lives that require a minimal component of various manifestations of strength (maximum strength, power and strength endurance). Therefore, both strength and muscle (quality rather than quantity) are physical function related parameters that need to be taken care of in the quest for achieving a healthy aging phenotype.
These issues are even more important when we note that as of 1st of October 2016, in the tenth revision of the International Classification of Diseases (ICD-10), sarcopenia has been classified as a disease by WHO and has its own code (M62.84). This should lead to increased availability of diagnostic tools and increased enthusiasm for the pharmaceutical industry to develop drugs to combat sarcopenia6. But in my opinion, this also represents a great opportunity for exercise professionals to be able to help fighting this disease, as strength training (properly oriented of course) will be the most potent stimulus in its prevention and treatment.
Pedro Correia
References:
- Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Comprehensive Physiology. 2012;2(2):1143-1211. doi:10.1002/cphy.c110025.
- GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet, 2016; 388(10053):1659-1724.
- Beard JR, Officer A, de Carvalho IA, et al. The world report on ageing and health: A policy framework for healthy ageing. Lancet 2016;387:2145e2154.
- English KL, Paddon-Jones D. Protecting muscle mass and function in older adults during bed rest. Current Opinion in Clinical Nutrition and Metabolic Care. 2010;13(1):34-39. doi:10.1097/MCO.0b013e328333aa66.
- National Center for Injury Prevention and Control of the Centers for Disease Control and Prevention. Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs 2nd edition. Atlanta: 2015.
- Anker SD, Morley JE, von Haehling S. Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle. 2016 Dec;7(5):512-514. Epub 2016 Oct 17. PubMed PMID: 27891296; PubMed Central PMCID: PMC5114626.
We often hear reports from people who spend hours and hours in the gym and remain the same. They do not lose fat, do not gain lean mass, do not gain strength, nor improve their functional capacity. They simply do not evolve. We also have those who rely only on the traditional weight training component to lose weight and yet not always have results, regardless of the diet they follow.
So, what is the secret for having results? Program design and professional supervision may be more important than you think.
In a study conducted by Bea et al. (2010), the authors investigated the association of exercise frequency and volume (total weight lifted on the military press and squat exercises) with changes in body composition in postmenopausal women who participated in a progressive strength training program for six years.
The women were divided into three groups: one group did strength training during this period, one started strength training after one year and the third (control group) did nothing. The training programs were supervised by professionals and involved motivational strategies to increase adherence. The training program consisted of eight exercises (based on free weights and machines) and was done three times a week, progressively.
The results showed that the group that did nothing (control group) gained weight and fat over the six years, suggesting something that everyone should already know: if nothing is done, we will get fatter and weaker with each passing day.
But there is something more interesting to highlight. The authors analyzed the relationship between body fat and increased squat load and found that the women who gained the most strength had better control of their weight and body composition over time! This means that if you are always doing the same program without managing training variables and principles, stagnation is what will happen.
So, what we have to tell you is that if you are part of that package that spends hours in the gym, between exercise machines, selfies and talking to your partner, then you are certainly not on your way to good results. We know that the socialization part is important and should not be ignored, we simply believe that it must be well managed! The key is knowing how to clearly distinguish what is training and what is ‘’going to the gym’’. And more training time is merely a quantitative indicator, not a quality indicator.
Enjoy your training!
Pedro Correia
References:
Bea JW, Cussler EC, Going SB, Blew RM, Metcalfe LL, Lohman TG. Resistance Training Predicts Six-Year Body Composition Change in Postmenopausal Women. Medicine and science in sports and exercise. 2010;42(7):1286-1295. doi:10.1249/MSS.0b013e3181ca8115.
Check Part 1 HERE and Part 2 HERE
Implications and practical applications of calorie restriction and intermittent fasting
And now … can the practice of calorie restriction (CR) or fasting have therapeutic value in humans? As noted earlier (Part 1), randomized controlled trials in humans studying the effects of CR and fasting in humans are scarcer. It is not easy to find volunteers to subject themselves to the “discomfort” of eating less food.
Just an aside …
Changing something in someone’s diet can be a daunting task! In fact, and based on my experience, people are generally highly resistant to changing whatever their eating patterns are and tend to defend them tooth and nail! They elaborate the most varied rationales (and very sophisticated sometimes … like the typical “but my grandfather is 90 years old and always ate this and that”) to justify the intake of certain foods that, essentially, they are just used to or like eating. Nutrition is like a religion for some, believe me …!
Back to human studies …
The other practical reason for the lack of controlled randomized human trials on the effects of CR or fasting to study its effects on life expectancy and the incidence of “age-related diseases” is that human life expectancy is long. However, some randomized controlled trials in humans point to clear benefits of CR practice in certain populations. Listed below are some of these studies, type of intervention and significant effects observed.
• Wang et al. (2013)
- Sample: obese individuals.
- Intervention: 5 days of 30% CR (low-fat / high-carb or high-fat / low-carb) after isocaloric diet period.
- Significant results:
- CR diets decreased fasting insulin and leptin levels by increasing free fatty acid levels (indicating mobilization of fat stores);
- Insulin sensitivity did not improve significantly (perhaps due to the short 5-day period), however muscle insulin signaling (in response to insulin) increased only in the low-fat / high-carb diet subjects. Note that this effect on insulin signaling in response to the low-fat / high-carb diet (rather than the high-fat / low-carb diet) may represent only a transient adaptive response due to the higher glycemic load in the diet. The short duration of the study does not allow the conclusion of a sustained improvement in insulin regulation.
- Kitzman et al. (2016)
- Sample: elderly obese individuals (67 ± 5 years) with heart failure.
- Intervention: 20 weeks of CR (350-400kcal / day deficit) with or without exercise (1 hour walking 3 days per week).
- Significant results:
- Both CR and exercise (separately) increased aerobic capacity (indicated by increase in VO2 peak), with even greater effects if combined;
- Both CR and exercise (separately) improved body composition (fat loss) with even greater effects if combined;
- CR (but not exercise) reduced the inflammatory marker C-reactive protein (CRP) and correlated with weight loss.
- Snel et al. (2012)
- Sample: obese individuals with type 2 diabetes mellitus (T2DM) and insulin-dependent.
- Intervention: 16 weeks of CR (450kcal / day) with or without exercise (1 hour + 4 30-minute sessions on a cycle ergometer per week).
- Significant results:
- Both CR and exercise improved fasting glucose, insulin and glycosylated hemoglobin (HbA1c) levels;
- The RC + exercise group lost more fat and waist circumference compared to the CR group only;
- Both CR and exercise increased insulin receptor expression and signaling (revealed by muscle biopsy) as well as peripheral insulin sensitivity.
- Pedersen et al. (2015)
- Sample: overweight or obese, non-diabetic individuals with coronary artery disease.
- Intervention: 12 weeks of CR (800-1000kcal / day) with or without exercise (3 days / week interval aerobic sled).
- Significant results:
- Separately, CR was superior to exercise in weight loss, fat mass and waist circumference, as well as fasting blood glucose, insulin sensitivity and glucose tolerance. However, CR led to better results combined with the exercise program.
- Razny et al. (2015)
- Sample: non-diabetic obese individuals
Intervention: 3 months CR (1200-1500 kcal / day) with or without 1.8 g / day omega-3 fatty acids (in a 5: 1 DHA / EPA ratio).
- Significant results:
- CR with or without omega-3 supplementation resulted in similar decrease in body weight and fat mass;
- CR had a superior positive effect on triglyceride and insulin levels when combined with omega-3 supplementation;
- Sample: non-diabetic obese individuals
RC + omega-3 (but not only CR) improved indicators of insulin resistance (HOMA index).
- Prehn et al. (2016)
- Sample: postmenopausal obese women.
- Intervention: 12 weeks CR (<800kcal / day) followed by 4 weeks on an isocaloric diet or 16 weeks on an isocaloric diet (control group). Recommendation to increase physical activity per week.
- Significant results:
- CR (but not the isocaloric diet) resulted in better scores on memory performance tests;
CR (but not the isocaloric diet) resulted in improved glycemic control and HbA1c levels;
- CR-induced increase in cerebral gray matter density was negatively correlated with glucose levels.
- CR (but not the isocaloric diet) resulted in better scores on memory performance tests;
Recommendations and Conclusions
In fact, CR or fasting interventions do indeed appear to have clear therapeutic utility in improving health parameters related to obesity, inflammation, insulin resistance, oxidative stress, and cardiac function. It is important to note that just reducing the amount of food you eat may not be enough and perhaps not recommended. Such a simplistic and long-term intervention can result in nutritional deficits and thereby boycott putative positive health outcomes. It is therefore important to monitor and ensure adequate nutrient levels through supplementation and / or in choosing nutritionally dense foods. Also noteworthy are the positive synergistic effects that CR seems to have when combined with exercise (Snel et al., 2012; de Luis et al., 2015; Kitzman et al., 2016), which may be prescribed concomitantly. In this context, a very mild CR intervention (e.g. 10% deficit) or short intermittent fasting periods (> 14 hours and does not need to be daily) combined with exercise may have very positive effects and are likely to have higher compliance compered to more aggressive fasting or CR interventions.
Of course, severe and prolonged CR with no exercise (especially strength training) can induce lean mass loss that is highly undesirable if the goal is to improve health. Once again, and as with almost everything, the secret lies in the right dosage! In certain populations such as pregnant women (or women trying to conceive) and young growing individuals, prolonged CR interventions should be avoided as they may compromise development. However, I emphasize again that the most important thing is not to ingest “calories” but ingest “nutrients”! In older individuals with sarcopenia, CR should perhaps be avoided, although the most determining factors for reversing sarcopenia are strength training and adequate protein intake (which should be higher for older individuals (> 2g / kg bodyweight).
Regarding the specific case of intermittent fasting (note: the focus of this article is not to discuss the use of intermittent fasting as a fat loss and / or maintenance strategy or muscle mass gains in the sports context, but rather its potential for general health benefits) although few, the available randomized controlled trials in humans indicate that intermittent fasting do offer beneficial effects similar to those of constant CR and perhaps is easier to implement (Donati et al., 2008; Marzetti et al., 2009; Alirezaei et al., 2010; Arum et al.; 2014; Godar et al., 2015). Irregular fasting episodes (e.g. not eating breakfast once or twice a week on non-training days) can not only be a strategy easy to implement strategy as a mean to control total weekly calories ingested, and it also has positive hormonal effects is mediated by some of the mechanisms described above. “Hormesis” is defined as a mild stressor that is beneficial to health, stress resistance, growth and longevity. It results from exposure to an “adequate” dose of a stressor. CR or fasting (or exercise) is something that we are evolutionarily designed to tolerate, and which at the right dose gives us benefits and greater resilience. The occasional stress of not eating can be a “healthy discomfort”!
Until next time!
Nuno Correia
What mechanisms underlie the effects of calorie restriction or intermittent fasting on longevity and “age-related diseases”?
But after all what is “getting old” … and why …?
Aging has been characterized by several authors as a process of progressive deterioration of molecular, cellular and tissue structures and functions that is conditioned by genetic and environmental factors (Hu & Liu, 2014). This multifactorial and complex process resulting from this progressive loss of function makes the individual more vulnerable to disease and ultimately leads to death. The main determinants (resulting from genetic predisposition and environmental factors) that characterize the aging process at the cellular level have been identified as: free radical damage; mitochondrial dysfunction results in an accumulation of reactive oxygen species (ROS) and consequent oxidative stress; decrease and inefficiency of autophagy (an evolutionarily conserved process of recycling and “cellular waste removal” that is essential for cellular integrity, more details a bit ahead); changes in hormone-related signaling processes such as type 1 insulin-like growth factor (IGF-1), insulin and growth hormone; change in cholesterol and glucose metabolism; telomere shortening (Testa et al., 2014).
Now it seems that the aging process is indeed multifactorial. Probably the various aging theories (see part 1) are correct! In general, molecular processes are becoming more inefficient, slower and the system is progressively moving towards entropy. However, it seems that knowing the autophagy process (whose decline is associated with aging) may offer a “new” perspective on aging. Autophagy (or “self-digestion”) has been defined as an evolutionarily conserved (normal and important) catabolic process characterized by degradation in the lysosomes (cell organelle that functions as a “litter”) of damaged organelles, “defective” proteins and intracellular pathogens (Lavallard et al., 2012). Autophagy provides macromolecule degradation and recycling, not only providing new nutrients and energy during energy restriction (during calorie restriction or fasting), but also preventing the accumulation of cell metabolism by-products and protein aggregates in the cytoplasm. Therefore, autophagy is a protective and essential process for cellular homeostasis (Rubinsztein, Mariño & Kroemer, 2011) (note: rest assured that autophagy will “eat all the muscles” for a few hours without eating. That simply does not happen!). In fact, several authors have pointed deficient autophagic capacity as an important mediator of cellular senescence and consequent occurrence of “diseases or characteristics of old age” such as cardiovascular and neurodegenerative diseases; oxidative stress; weak immune system; chronic inflammation; osteoporosis; sarcopenia; diabetes; obesity; cancer (Pallauf & Rimbach, 2013; Pyo, Yoo & Jung, 2013). Specifically, reviews of mechanistic animal studies have indicated that loss of function in autophagy-related genes has resulted in intracellular accumulation of defective proteins and organelles and consequently in the acceleration of aging, while promoting autophagic activity increased life expectancy (Yen & Klionsky 2008)
(Note: Autophagy mechanisms have been in the mainstream news since 2016 with the Nobel Prize in Medicine 2016 awarded to the Japanese biologist Yoshinori Ohsumi. Their findings in autophagy mechanisms point in the direction that this cellular cleaning and recycling process is essential to prevent neurodegenerative and other diseases. This is the LINK for the news article).
Overall, and since the first rat studies by Dr. Clive McCay in 1935, calorie restriction has been extensively reviewed and recognized as a “potent” anti-aging strategy! Interventions in various types of animal species (from invertebrates to larger mammals such as primates) have shown that calorie restriction (without malnutrition) not only increases life expectancy (average and maximum), but delays the onset of so-called “age-related diseases ”(Martin, Mattson & Maudsley, 2006; Xiang & He, 2011; Lee & Min, 2013; Kitada & Koya, 2013b; Szafranski & Mekhail, 2014; Testa et al., 2014). The intermittent fasting regime (nothing more than another calorie restriction strategy as described in part 1 of this article) seems to offer the same kind of benefits (Martin, Mattson, & Maudsley, 2006; Robertson & Mitchell 2013).
Now the mechanisms by which calorie restriction or fasting induce health benefits appear to be (to a large extent) related to this antagonistic relationship between insulin signaling and autophagy. It is easy to understand, being autophagy a catabolic process (essential, normal and protective, I highlight that again) and the activation of insulin signaling pathways an anabolic process (equally important and essential in protein synthesis, insulin is not the “villain”), when one of these pathways is activated the other will be inhibited. Practically speaking, fasting activates the autophagy “machinery” and eating a meal (mainly containing protein and / or carbohydrates) activates the insulin signaling “machinery”. What seems to be essential is in fact that there are periods that allow the process of elimination and recycling provided by autophagy, and for this to happen it is necessary not to eat for a while. If there is no “room” for this process, due to constant food intake, it may lead to constant and “aberrant” insulin signaling state which may lead to many diseases that are usually associated with poor glucose and insulin metabolism which make the most of the so-called “age diseases”.
(Warning: the “less nerds“ should skip next paragraph)
Briefly, some of the mechanisms identified in animal studies that appear to underlie the health benefits induced by caloric restriction or intermittent fasting through regulation of autophagy and insulin pathway signaling are: 1) Inhibition of insulin / IGF-1signaling (due to the decrease in circulating amino acids and glucose) and its target pathways protein kinase B (PKB) / mammalian target of rapamycin (mTOR) ; 2) Activation of the sirtuin 1 pathway (SIRT1) due to the increase in NAD + / NADH ratio, which targets include activation of adenosine monophosphate protein kinase (AMPK), forkhead box O (FOXO) transcription factors, proliferator- activated gamma receptor-1-alpha coactivator (PGC-1α) (a mitochondrial biogenesis factor), and inhibition of the pro-inflammatory transcription factor NFkB; 3) Activation of the AMPK pathway due to the intracellular increase of the AMP / ATP ratio, which in turn induces up-regulation of FOXO and PGC-1α transcription factors and inhibition of the PKB / mTOR pathway. (Martin, Mattson & Maudsley, 2006; Han & Ren 2010; Rubinsztein, Mariño & Kroemer, 2011; Yen & Klionsky, 2008; Xiang & He, 2011; Pallauf, & Rimbach, 2013; Pyo, Yoo, & Jung, 2013; Hu & Liu, 2014; Szafranski & Mekhail, 2014; Amigo & Kowaltowski, 2014; Testa, G. et al., 2014; Madeo et al., 2015).
In humans, despite the smaller abundance of randomized controlled trials (for the reasons mentioned in Part 1 of this article), several reviews of intervention and observational studies (Yen & Klionsky, 2008; Marzetti, E. et al., 2009; Han & Ren 2010; Robertson & Mitchell, 2013; Testa et al., 2013; Madeo et al., 2015; Fan et al., 2016) indicate that the putative health benefits induced by calorie restriction or intermittent fasting are based on the same mechanisms related to insulin pathway signaling and regulation of autophagy. Some pointed benefits include: longer healthy longevity; better lipid profile; controlled blood pressure; optimization of diastolic and systolic function; better homeostatic control of insulin and glucose; better sensitivity to insulin and glucose; lower incidence of neurodegenerative diseases; lower adiposity; better mitochondrial biogenesis in the skeletal muscle; higher antioxidant capacity; lower levels of ROS and oxidative stress.
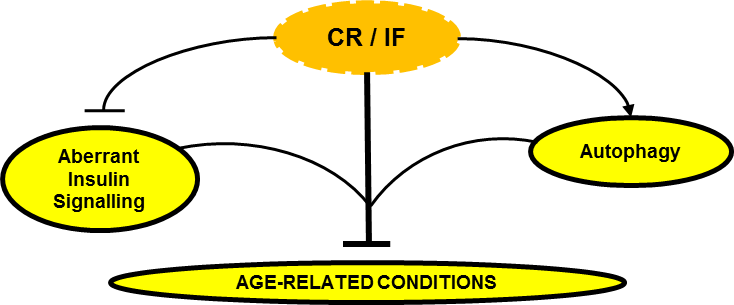
Can Calorie Restriction / Intermittent Fasting (CR / IF) alleviate age-related disease by regulating “aberrant” insulin signaling and autophagy?
In conclusion, the effect of caloric restriction or intermittent fasting on the regulation of insulin signaling and autophagy seems to emerge as a central regulatory axis that deserves attention (at least from me).
In the third part of this article I will then discuss what may be practical implications and applications of calorie restriction or fasting. Should we all do calorie restriction? Permanently? For how long? How much? What stage of life? Under what health conditions? Is the “intermittency” factor that delivers the best benefits?
Stay around!
Nuno Correia
References:
Amigo, I. & Kowaltowski, A.J., 2014. Dietary restriction in cerebral bioenergetics and redox state. Redox Biology, 2(1), pp.293–304.
Dröge W., 2009. Avoiding the First Cause of Death. New York, Bloomington. iUniverse, Inc.
Fan, J. et al., 2016. Autophagy as a Potential Target for Sarcopenia. Journal of Cellular Physiology, 231(7), pp.1450–1459. [Epub 2015 Dec 10].
Han, X. & Ren, J., 2010. Caloric restriction and heart function: is there a sensible link? Acta pharmacologica Sinica, 31(9), pp.1111–1117.
Hu, F. & Liu, F., 2014. Targeting tissue-specific metabolic signaling pathways in aging: the promise and limitations. Protein & cell, 5(1), pp.21–35.
Lavallard, V.J. et al., 2012. Autophagy, signaling and obesity. Pharmacological Research, 66(6), pp.513–525.
Lee, S.-H. & Min, K.-J., 2013. Caloric restriction and its mimetics. BMB reports, 46(4), pp.181–7.
Lee, S.-H. & Min, K.-J., 2013. Caloric restriction and its mimetics. BMB reports, 46(4), pp.181–7.
Lindeberg, S., 2010. Food and Western Disease: Health and Nutrition from an Evolutionary Perspective. Oxford, United Kingdom: Wiley-Blackwell.
Madeo, F. et al., 2015. Essential role for autophagy in life span extension. Journal of Clinical Investigation, 125(1), pp.85–93.
Martin, B., Mattson, M.P. & Maudsley, S., 2006. Caloric restriction and intermittent fasting: two potential diets for successful brain aging. Ageing research reviews, 5(3), pp.332–53.
Masoro.E. L., 2002. Caloric Restriction: A Key to Understanding and Modulating Aging. Texas, USA: ELSEVIER.
Pyo, J.O., Yoo, S.M. & Jung, Y.K., 2013. The interplay between autophagy and aging. Diabetes and Metabolism Journal, 37(5), pp.333–339.
Robertson, L.T. & Mitchell, J.R., 2013. Benefits of short-term dietary restriction in mammals. Experimental gerontology, 48(10), pp.1043–8.
Rubinsztein, D.C., Mariño, G. & Kroemer, G., 2011. Autophagy and aging. Cell, 146(5), pp.682–695.
Rubinsztein, D.C., Mariño, G. & Kroemer, G., 2011. Autophagy and aging. Cell, 146(5), pp.682–695.
Szafranski, K. & Mekhail, K., 2014. The fine line between lifespan extension and shortening in response to caloric restriction. Nucleus, 5(1), pp.56–65.
Testa, G. et al., 2014. Calorie restriction and dietary restriction mimetics: a strategy for improving healthy aging and longevity. Current pharmaceutical design, 20(18), pp.2950–77.
Xiang, L. & He, G., 2011. Caloric restriction and antiaging effects. Annals of Nutrition and Metabolism, 58(1), pp.42–48.
Yen, W.-L. & Klionsky, D.J., 2008. How to live long and prosper: autophagy, mitochondria, and aging. Physiology (Bethesda, Md.), 23(70), pp.248–262.
CAN CALORIE RESTRICTION OR INTERMITTENT FASTING HELP PREVENT “AGE-RELATED DISEASES” AND LIVE LONGER? – PART 1
Introduction
In this article I will look into the possibility of calorie restriction or intermittent fasting, which is just an alternative strategy to induce a caloric deficit, effective nutritional therapeutic strategies to prevent, alleviate or even eliminate some of the so-called “age-related diseases”, thus contributing for a better and longer life. It is important to note that most studies on the effects of calorie restriction or intermittent fasting (or intermittent calorie restriction) on life expectancy are mechanistic, and conducted in animal and / or in vitro models. It is understandable that there are fewer human intervention studies in this area. If we think about it, it is not easy to conduct studies with humans on calorie restriction to study its effects on life expectancy and the incidence of “age-related diseases”. Not only it is not easy to recruit people to voluntarily incur in a calorie restriction period, it is also not practical to study in humans (in a randomized controlled manner) the effects of calorie restriction or fasting on life expectancy, because they simply “live a long time”. ” In order to obtain timely results, it is essential to conduct studies on species with a shorter life expectancy. However, observational studies and some human intervention studies (discussed later) appear to confirm the same health benefits and molecular mechanisms as those observed in animals.
It should also be noted that, in the experimental context, caloric restriction is defined as “reduced food intake without malnutrition”. In other words, nutritional interventions imply a 10-40% reduction in daily caloric requirements in which only calories, and not nutrients, are restricted (in most controlled studies this is ensured with vitamin and mineral supplementation) (Kitada & Koya, 2013b; Robertson & Mitchell, 2013). This notion is important! Caloric deficit does not imply nutrient deficit and caloric surplus does not imply that nutrient requirements are met. Intermittent fasting will be no more than an alternative method of calorie restriction in which food intake is restricted for a certain period of time (usually 16 to 24 hours) followed by an unrestricted intake period and has been touted as producing beneficial health effects similar to more constant calorie restriction protocols (Martin, Mattson, & Maudsley, 2006; Robertson & Mitchell 2013).
Part 1
Should we accept being “sick” just because we get older?
It is recurrent to hear that the disease is something that “comes with the age package.” In fact, getting older is a drag! The general perception of a progressive decline of all our capabilities as we age is, unfortunately, not an illusion. There are several theories about aging. While certainly a very interesting topic, a detailed description of the various theories of aging is not the purpose of this article. These are some of mechanisms underlying the aging process which are generally pointed out as the main ones:
- The “Hayflick limit” (phenomenon discovered by Leonard Hayflick) determines that human cells have a replication limit number, after which they become senescent. Telomeres (i.e. a kind of protective “helmets” at the end of each chromosome) become progressively shorter with each cell division (Shay & Wright 2000). However, DNA methylation (an essential and repairing process consisting of the addition of methyl groups to DNA and which can be promoted by the abundance of dietary methyl donors for example) is said to be protective of telomere length and that way to postpone cell death and aging. For example, in animal models, hypomethylation of the enzyme telomerase reverse trancriptase has led to the preservation of leukocyte telomere length (Zhang et al. 2003; 2014). In this example, it is plausible to infer that delaying leukocyte senescence (through methylation and consequent telomere length conservation) may contribute to a stronger immune system and thus positively influence longevity.
- This theory suggests that unresolved chronic inflammation induces the human organism not to allocate resources for the functioning of other body functions (as they are permanently allocated to unresolved inflammation) and thus leading to early aging of various organs and tissues, and the early onset of “age-related diseases”.
- This theory, originally proposed by Dr. Denham Harman in 1956, is based on the premise that the aging process is mediated by free radical damage. Theoretically, by reducing free radical accumulation (e.g. reactive oxygen species) and at the same time increasing the antioxidant capacity of the organism (increasing glutathione, and antioxidant enzymes such as SOD and catalase), tissue damage can be prevented (by slowing down aging process) and to prevent the occurrence of “age-related diseases” and consequently contribute to increase functional longevity (Harman, 1988; 2006).
Very well, getting older is inevitable! We already know that. However, if we give it a little thought, all the mechanisms mentioned have an environmental root, that is, we can, to some extent, control them through decisions that we make every day. Namely decisions about what we eat and how we move. And this is good news! It is in fact in our hands to slow down the process of senescence and prevent the onset of the so-called ‘’age-related diseases’’. Note that if for us (Westernized world) it is statistically “normal” to grow old with diabetes, hypertension, cancer, dementia, sarcopenia, osteoporosis, cardiovascular disease, insulin resistance, obesity and chronic inflammation (because the population studied incurs in a lifestyle that leads to disease), in other contemporary (non-Westernized) populations such diseases are rare or even non-existent. In this context, I invite the reader to consult what I consider to be one of the best books I know about nutrition and lifestyle, and its relation to the incidence of so-called “Western” diseases: Food and Western Disease: Health and Nutrition from an Evolutionary Perspective by Staffan Lindeberg. In fact, if we want to aim at maximizing health and lifespan potential, we should not just look at what is ‘’normal’’ in a given population, because that may be a sick population. Rather, we should look for what is “biologically normal” for a human being! A species that is designed (evolutionarily) to deal with a range of environmental stimuli that include certain levels of physical activity, nutrition, sun exposure and sleep. And, although aging is a normal process, it should not be “biologically normal” to age with chronic disease.
In this context, the Okinawa Centenarian Study is also frequently cited. The Okinawan population has the highest ratio of (healthy) centenarians on the planet (50 / 100,000 vs 10-20 / 100,000 in the USA) and as such is of greatest interest to study the factors that potentiate this kind of longevity. One of the factors identified (in addition to an appreciable level of physical activity and social interaction) was the fact that populations over 70 eat about 11% of calories below (about 1785kcal / day, which is a very moderate level of calorie restriction) than would be recommended for maintaining body weight (according to the Harris-Benedict equation), however on a nutrient-rich diet (Wilcox et al., 2006).

What we can do to live longer and better is one of my main interests. As I mentioned, our choices regarding the type of exercise, food we eat and other lifestyle factors can affect how long we live and, perhaps most importantly, how healthy and functional we live. In Part 2 of this article I will discuss some mechanisms by which nutritional interventions such as calorie restriction or intermittent fasting can lead to health benefits. And in Part 3 I will address the possible implications and practical applications of the practice of calorie restriction or fasting, as well as which populations can benefit most from these nutritional strategies and whoshould avoid them.
Stay around!
Nuno Correia
References
Dröge W., 2009. Avoiding the First Cause of Death. New York, Bloomington. iUniverse, Inc.
Harman D., 1988. Free radicals in aging. Mol Cell Biochem. Dec; 84(2), pp.155-161.
Harman D., 2006. Free radical theory of aging: an update: increasing the functional life span. Ann N Y Acad Sci. May;1067, pp.10-21.
Kitada, M. & Koya, D., 2013b. SIRT1 in Type 2 Diabetes: Mechanisms and Therapeutic Potential. Diabetes & metabolism journal, 37(5), pp.315–25.
Lindeberg, S., 2010. Food and Western Disease: Health and Nutrition from an Evolutionary Perspective. Oxford, United Kingdom: Wiley-Blackwell.
Martin, B., Mattson, M.P. & Maudsley, S., 2006. Caloric restriction and intermittent fasting: two potential diets for successful brain aging. Ageing research reviews, 5(3), pp.332–53.
Masoro.E. L., 2002. Caloric Restriction: A Key to Understanding and Modulating Aging. Texas, USA: ELSEVIER.
Robertson, L.T. & Mitchell, J.R., 2013. Benefits of short-term dietary restriction in mammals. Experimental gerontology, 48(10), pp.1043–8.
Shay J.W., Wright W.E. 2000. Hayflick, his limit, and cellular ageing. Nat Rev Mol Cell Biol. Oct;1(1), pp.72-76.
Zhang D. et al., 2013. Homocysteine-related hTERT DNA demethylation contributes to shortened leukocyte telomere length in atherosclerosis. Atherosclerosis. Nov; 231(1), pp.173-179.
Zhang D.H., Wen X.M., Zhang L. & Cui W., 2014. DNA methylation of human telomerase reverse transcriptase associated with leukocyte telomere length shortening in hyperhomocysteinemia-type hypertension in humans and in a rat model. Circ J. 78(8), pp.1915-1923.
Wilcox D.C. et al., 2006. Caloric restriction and human longevity: what can we learn from the Okinawans? Biogerontology 7, pp.173–177.
Strength training has been recognized as the strategy of choice to stay more functional and live longer. The benefits of strength training are in fact ubiquitous and positively affect the various biological systems that tend to decline with age, namely systems related to neuromuscular, cardiovascular and cognitive functions.
It has been observed that strength training programs in which the included exercises are performed at higher intensities (> 80% of maximum intensity) or with lighter loads but performed explosively tend to produce better results compared to training protocols where exercises are performed at lower intensities and / or non-explosively (Mendonça et al., 2016a). The magnitude of the load used (i.e. heavy or lighter but performed explosively) are especially relevant for older populations. Why? Because aging is associated with the loss of Type II muscle fibers, which are responsible for producing maximal strength (e.g. lifting a weight and not being able to lift it again in the next minutes or hours) or as explosive strength (e.g. moving an object or your own bodyweight at maximal speed). Now, the overwhelming majority of daily life movements are ballistic in nature (i.e. fast, short duration movements) and often for the purpose of moving relatively heavy objects for a short period of time. Therefore, it is not surprising that a training program that includes exercises that imply moving heavy loads and / or loads moved explosively is more effective in “preparing” people for everyday activities.
Training at higher intensities in a training program based on fundamental movement patterns (squatting, pushing, pulling, loading and lifting objects off the ground) makes people less vulnerable to falls and “tweaks”, and at the same time more able to recover from such incidents should they occur.
Train hard and smart! A structured training program that respects the principle of progressive overload is more valuable than a program that always keeps you within the comfort zone. Be as active as you can get during the day but IF TRAINING AT GYM DO NOT WASTE YOUR TIME, AND REALLY TRAIN! Seriously, it works!
Good lifting! ?
References
Mendonca, G. V. et al., 2016a. Impact of Exercise Training On Physiological Measures of Physical Fitness in the Elderly. Current aging science, 9(3).
The self-reported prevalence of shoulder pain is estimated to be 16-26% and this is the third most common cause of musculoskeletal disorder on consultation (see reference below). Physical factors such as your exercise habits and repetitive (low and high intensity) movements in inappropriate positions can result in injury or chronic pain.
For these reasons, at The Strength Clinic, we consider that there are four fundamental pillars in the way your shoulder should function:
1) Breathing – Breathing properly is very important to maximize performance. A normal person breathes on average more than eight million times a year, and it is likely that he/she does not do it efficiently. Most people use only a small percentage of the body’s ability to draw oxygen from the air into the lungs because they tend to breathe only through the upper respiratory tract (apical breathing), instead of breathing deeper from the most efficient respiratory muscle we have, the diaphragm.
2) Posture – Although overrated most of the time, each individual’s posture may have an influence on the onset of injuries and in the prevalence of chronic pain. Especially when we talk about activities with high impact / high loads (in which biomechanics assumes a fundamental role) and the daily habits of movement that each person has. A poor posture is usually the result of various structural, muscular and joint imbalances. However, it should be noted that our body has a huge adaptive capacity and that the lack of quality movement is probably the main problem. Contrary to what you may think there are no perfect postures!
3) Grip Strength – There is a phenomenon called irradiation, so the higher the grip strength, the greater the activation of nerves and muscles along the kinetic chain. Therefore, there will be an increase in neurological efficiency, and we will have the rotator cuff muscles (supraspinatus, infraspinatus, teres minor, subscapularis) firing the way they should, which is as dynamic stabilizers centering the head of the humerus on the joint, and not otherwise inhibited due to lack of grip strength. The hands are closely linked with the functioning of the physiological and neurological system but unfortunately this is a phenomenon largely ignored in today’s training programs.
4) Joint Position – Rotator cuff training alone will not ensure the functional health of your shoulder. The stability of the shoulder blades, which depends on the mobility of the thoracic spine, is critical to ensure that the glenoid cavity is well positioned for the applied forces. The stability of the hips and trunk is also necessary to serve as a foundation for the position and functioning of the shoulder blades. In other words, if your central axis control is weak, your shoulder blades are most likely to be drawn into unfavorable positions and this will impair force transmission.
Therefore, any strategy aimed at improving the functionality of the shoulder should consider these four pillars because a seemingly strong shoulder is not necessarily a stable shoulder and it is stability that must precede force production.
Pedro Correia
References
Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ: British Medical Journal. 2005;331(7525):1124-1128.
For many years, breast cancer survivors have been told not to lift anything heavier than a handbag because of the risk of lymphedema (swelling / edema caused by accumulation of lymphatic fluid in the tissues of the body’s surface). This accumulation of lymphatic fluid (lymph) arises as a consequence of changes in the lymphatic system due to surgery and / or radiotherapy to the lymph nodes in the axilla and surrounding areas.
In this regard, it is recommended that women should ask for help with shopping bags, should avoid lifting or carrying children, and should only engage in exercise modalities such as walking, swimming and other light aerobic activities – these are the general recommendations. However, a study published in the New England Journal of Medicine in 2009 (see reference below) has shown that lifting weights can be a substantial aid to women with or at risk of developing arm lymphedema.
In this study the researchers recruited 141 breast cancer survivors with stable arm lymphedema and divided the sample into two groups – one group did strength training and the other did not change their exercise routine. These were the conclusions of the authors of the study: “in breast-cancer survivors with lymphedema, slowly progressive weight lifting had no significant effect on limb swelling and resulted in a decreased incidence of exacerbations of lymphedema, reduced symptoms, and increased strength.”
So, the main question here is not whether women who suffer from this condition may or may not lift weights but HOW they should do it to improve their condition. Again, the critical component is the program design, and this is one of our distinctive competencies at The Strength Clinic.
Train smart.
Pedro Correia
References
Schmitz KH, Ahmed RL, Troxel A, Cheville A, Smith R, Lewis-Grant L, Bryan CJ, Williams-Smith CT, Greene QP. Weight lifting in women with breast-cancer-related lymphedema. N Engl J Med. 2009 Aug 13;361(7):664-73. doi: 10.1056/NEJMoa0810118. PubMed PMID: 19675330.
If you still exercise to “burn calories,” you have not yet realized the purpose of a physical training program and the importance that movement has in our lives. The least important thing about exercise is the number of calories you burn! And that’s what I’ll try to explain in this article.
The power of exercise goes far beyond calorie burning, caloric expenditure is just a (nice) side effect of the type of exercise we do. Exercise consists of potentiating the release of powerful molecules and hormones that “talk” to our body’s organs (it’s not just food that has this kind of influence), and that determines what’s going to happen. And usually, the higher the intensity, the more beneficial the hormonal response.
Therefore, a well-designed physical training program has more to do with increasing energy levels, movement precision, vigor, muscular strength, mobility, agility, speed, work capacity and with an improved hormonal profile.
The Calorie Fever
I still see a lot of people worried about the calories in their food, the calories they burn when they exercise, the calories they consume each day, and I ask: How did we get here? What kind of message is being propagated that made people so obsessed with calories? Is calorie counting that important? Let’s see.
In order to discover the amount of energy in food, scientists burn food samples in a bomb calorimeter. And, to my knowledge, a bomb calorimeter does not share the same physiology and genetic makeup as a human being. As far as I know, a bomb calorimeter does not depend on the functioning of the various systems in the human body which are the real players in the way energy is absorbed and used (examples: digestive, endocrine and nervous system). This way of thinking is most likely unsustainable and ineffective long-term. This way of thinking is too reductive and does not solve the main problem – people’s lack of education regarding the importance of what we eat throughout our lives. Is it just me who finds it strange that most people are more concerned about their cell phones, cars and computers than with the origin and composition of the food they eat?
In fact, just look around and you’ll acknowledge that this is not the path to follow!
It is true that if we have the goal of losing fat mass, we must create an energy deficit, that is, the balance between the amount of calories (energy) entering our body and the amount of energy (calories) burned, must be negative. That’s the number one rule in rigid weight loss programs and that’s why we see Biggest Loser contestants training several times a day.
(Note: I should remind you that the Biggest Loser is a contest in which the goal is to lose weight in the shortest time possible, it’s not a contest to see who gets out of there healthier – if this was the goal probably there was no audience).
However, there is a lot more to be said. There are good calories and bad calories. The foods we eat, besides having a certain number of calories (which can be very difficult to determine with accuracy and can be highly variable), also have different properties with respect to their composition of macronutrients (protein, fat, carbohydrates) and micronutrients (minerals, vitamins, phytochemicals). These bioactive properties and compounds are what makes the difference and what should be studied preferentially. In my way of looking at things, it is more logical to first check the functionality of food (i.e. how its nutrients work) and then look at its caloric density, which can also be more or less functional depending on the objectives, morphology and specific conditions of each individual.
(Note: If you still think low fat diets are the most suitable for weight loss check the following study published in 2003 in the New England Journal of Medicine here, where it was shown that people on a high-fat diet lost more weight as those on a low-fat diet, the diet generally recommended by leading health organizations. But, of course, adherence to the diet will be the most important factor).
Back to calories…
Because the absorption of these nutrients will depend on the functioning of our digestive system – which in turn is governed by the endocrine system (think of hormones) and the nervous system (think of neurotransmitters) – and the health of the organs involved in the digestion process (mouth, esophagus, stomach, pancreas, small intestine, large intestine, liver, gallbladder), it becomes easy to understand that the web of relationships in the human body is much more complex than simple calorie counting. Albert Einstein has a quote that fits perfectly here: “make everything as simple as possible, but not simpler.”
The Power of Exercise
Anyone that is minimally informed about exercise already knows that long distance aerobic training is not the best choice for improving body composition and may even have opposite effects (catabolic effects) due to the pronounced increase in cortisol levels.
This has been known for a long time but it’s always important to remember. This study published by Tremblay, Simoneau and Bouchard in 1994, showed that the group that did 15 weeks of interval training burned NINE TIMES more fat than the group that did aerobic training. And this was in half of the time period!
What you need to “burn calories” is to increase the intensity of your workouts for certain periods of time, it’s this type of stimulus that will increase your metabolism and accelerate fat loss. In this study, a 30-minute training session of metabolic resistance training caused a 38-hour increase in metabolism – the famous afterburn effect or EPOC (post-exercise oxygen consumption). Let’s put this into perspective. Let’s say you trained this way on Friday morning. With this training method your body will still be in a “fat burning” mode on Saturday night, when you’re having dinner with your friends or with your boyfriend / girlfriend.
And why do I insist on combining a good diet with good training? Because I’m aware of the evidence on this topic. This study from 1999 showed that those who did aerobic training and strength training on a low calorie diet burned 44% more fat than those who merely followed dietary guidelines. As I’ve been saying, diet is the most important component for those people who want to lose fat, however, once that aspect is assured, only strength training and interval training can actually bring your results to a higher level. In my opinion, the fact that this study was based on a low-calorie diet combined with aerobic training is limiting, but we have to bear in mind that these are usually the guidelines of the American College of Sports Medicine (ACSM). The guidelines are intended to facilitate nutritional guidance offered by practitioners, but unfortunately that is not what I have observed when I discuss these issues with some colleagues.
I think you have already realized that the type of training you do can be a great ally to put your body in an energy deficit and consequently in fat burning status. Now I will try to explain why this is the least important of all. Stay with me!
Like nutrition, physical exercise is key to improve health, performance and body composition. You’re probably tired of hearing this. But it’s not any kind of physical exercise that works. Doing hundreds of crunches to lose belly fat, using all the gym machinery, running 10 miles a day, doing Pilates twice a week and doing 100 power cleans in the shortest time possible is not enough. You can call it physical exercise if you want, but it’s not just this kind of physical exercise our body needs. A more comprehensive approach is needed.
We need Good Movement (we shouldn’t start running in the first place)
The concept of “move more for your health” is insufficient for our real needs and to improve quality of life. We need good movement, we need to acquire movement competency in the first place. I am talking about the ability to perform fundamental movements with good form. Fundamental movement patterns such as squatting, hinging, pushing, pulling, throwing, carrying, walking, running and jumping.
From my point of view, running should be the last step in this process and yet what we most frequently see is people running all crooked and with an obvious deficit in muscle strength. But the problem is not theirs, they are trying to do something for their health (and probably that’s all they know), the problem is that most of them are not aware that running is a skill, which requires preparation, practice and training. Cristiano Ronaldo did not become the best player in the World over night, it took many hours of training (in the field and in the gym) to reach this level. Although it’s relatively easy and affordable for anyone to put on their shoes and just go out for a run, running also requires preparation, practice and training (technical and physical).
It is necessary to have stability, mobility, strength (every step we take on the ground is subject to the action of gravity and the speed we run, generating reaction forces of 2 to 5 times our body weight), symmetry, quality of movement and good musculoskeletal health. Running to get healthy or fit is one of the greatest physical distresses on our body if we don’t have a solid foundation. First, you need to be in good shape to run. If you don’t hone good movement skills, you are more likely to get injured. According to the available literature, the incidence rate of injury in runners may exceed 90%, this is more than any other sport. Plantar fasciitis, stress fractures, patellar tendonitis and patellofemoral pain are just a few examples. Check this systematic review if you’re interested in learning more.
Again, don’t get me wrong, I’m not anti-running and I admire the effort and suffering capacity of all runners. I think we should all be able to run (by the way, that’s how we evolved as a species), the problem is that most people who run are not properly prepared to run and there are fundamental learning steps that should not be overlooked in order to prevent structural imbalances in the musculoskeletal system and injuries. Cleary the simplistic idea of “move more” is not enough.
A new way to look at training
Different types of training can affect the way our genes work and how they interact with our cells. With good training it’s possible to decrease chronic inflammation, improve insulin sensitivity, strengthen the cardiovascular system, improve lipid profile, slow down normal aging, burn fat (as we’ve seen in more detail above), increase confidence and self-esteem, increase energy levels, increase mental strength, improve a number of physical skills that we need for our daily life activities or sports practice (such as strength, stability, mobility, balance, speed, agility) and our different energy systems (ATP-CP, glycolytic, and oxidative). As we age, these skills naturally decline, but the fact is that with a more comprehensive training program it is possible to reverse and / or at least mitigate this decline.
Most people think that genes are the brain of the cell, they believe that if genes don’t tell you what to do, the cell dies. But if you remove the genes from the cell, the cell is still alive, eliminating waste products and behaving just like another cell. So, instead of genes being the brain of the cell, think of genes as your instruction / repair manual. When a worn part of the cell needs to be repaired or when new substances need to be produced, genes will give instructions for doing so.
Every cell in our body is surrounded by a fatty membrane, which is filled with thousands of receptors. These receptors receive information from different parts of the body and pass this information into the cell to form / encode new proteins, burn more or less fat, etc. (Note: this is why it’s important to eat good fats and avoid the hydrogenated fats present in most processed foods so that the cell membrane is more permeable to nutrient delivery.) It’s this membrane with receptors the cell command center so if we remove these membrane receptors, the cells die. This means that cell function is highly influenced by external factors, namely through hormones and other molecules that bind to these receptors.
These messenger molecules are not randomly created by our body, they are created according to our lifestyle, diet, thoughts, behaviors, temperature, light, sound and… our type of training. It’s possible to be born with some defective genes – for example BRCA 1 and BRCA 2, which increase the risk for breast cancer – but it’s these messenger molecules / hormones that will determine the degree of activation of these genes. Therefore, controlling these hormones means controlling the body.
(Note: Don’t you find it strange that almost 90% of health care costs is related to treat health conditions, while 80% of health problems / diseases arise as a consequence of our lifestyle and the environment we’re exposed to? Check this TED talk from Dan Buettner to realize why we are walking in the wrong direction).
High-intensity exercise is the one that induces a more favorable hormonal environment, with an increase in hormones such as testosterone, growth hormone and IGF-1, interleukins with an important role in inflammation (IL-6), muscle tissue maintenance (IL-15) and growing of new blood vessels (IL-8), lactic acid (which has the ability to keep us young by stimulating the release of testosterone and growth hormone) and nitric oxide, a vasodilator which plays a key role in regulating blood pressure, muscle strength and erectile dysfunction. Unfortunately, long running does not produce the same effects. Compound movements, which require a combination of strength and stamina, in short periods of time, are those that will put your muscles to “talk” more with your body. Burning calories is only a minor side effect when compared to the amount of hormones and other signaling molecules that influence how our body works.
To be clear, we are talking about intensity coupled with movement quality. Intensity coupled with bad movement will have the opposite effect: INJURY.
Conclusion
It’s urgent to give rise to a new mentality on training the movement skills that we will need throughout our lives. And this is a serious limitation of most group classes in conventional gyms. The instructors are obliged to follow a certain beat and choreography. Individualized feedback is almost non-existent. People don’t have time to understand or to learn the movements. And no one learns anything if they don’t know what it’s for, no one learns anything if they don’t understand how it’s supposed to feel and its practical implications. In addition, most machines in gyms annihilate the sensory and body perception that we, humans, need. We live in a three-dimensional world, in a world of constant adaptation and spatial exploration, so it makes no sense that machines and choreographies of group classes dictate the rules of our movement.
And why is it important to learn efficient movements? First, an efficient movement happens when a body is able to produce force through a coordinated action between the various body segments without energy leaks and demonstrating a natural ability to exploit maximum range of motion. Second, it’s movement that will allow you to play more time with your children, change the furniture at home, improve your day-to-day performance and your performance in your recreational activities.
Look at this type of training as the foundation, the support you need to get stronger, faster, smarter, more agile, more competent in a series of physical attributes that will allow you to perform better in the activities you enjoy doing. Would you like to start playing tennis? golf? volleyball? Would you like to start surfing? paddle board? weightlifting? powerlifting? dance? climbing? triathlon? Would you like to be faster when you play football with your friends during on weekends? Obviously, each modality has its specific abilities, but they all share the same foundation: human being’s adaptability capacity. To improve these specific skills safely, you first need to improve your fundamental movement patterns. And to sustainably keep improving these fundamental movement patterns, you need to train better and respect the developmental stages of each one.
To sum up, the great advantage of better training (and I remind you what we learned about the power of exercise, good movement and a new way of looking at training) is to improve your quality of life, maximize your performance and, above all, giving you the freedom and autonomy to choose the activity / sport that you always wanted to try but never had the courage or opportunity to start off.
Think about these things next time you go to the gym to walk on the treadmill with your headphones on and watch some TV series for 40 minutes while looking at the calories burned on the monitor and at the workouts or exercises other people are doing.
See you soon!
Pedro Correia
References
Berardi, J, Andrews, R. The Essentials of Sport and Exercise Nutrition. Certification Manual. Second Edition. Precision Nutrition Inc. (2013).
Björntorp P. Hormonal control of regional fat distribution. Hum Reprod. 1997 Oct;12 Suppl 1:21-5. Review.
Frederick F. Samaha, M.D., Nayyar Iqbal, M.D., Prakash Seshadri, M.D., Kathryn L. Chicano, C.R.N.P., Denise A. Daily, R.D., Joyce McGrory, C.R.N.P., Terrence Williams, B.S., Monica Williams, B.S., Edward J. Gracely, Ph.D., and Linda Stern, M.D. A Low- Carbohydrate as Compared with a Low-Fat Diet in Severe Obesity. N Engl J Med 2003; 348:2074-2081.
Gary D. Foster, Ph.D., Holly R. Wyatt, M.D., James O. Hill, Ph.D., Brian G. McGuckin, Ed.M., Carrie Brill, B.S., B. Selma Mohammed, M.D., Ph.D., Philippe O. Szapary, M.D., Daniel J. Rader, M.D., Joel S. Edman, D.Sc., and Samuel Klein, M.D. A Randomized Trial of a Low-Carbohydrate Diet for Obesity. N Engl J Med 2003; 348:2082-2090.
Houston, M. What your doctor may not tell you about Heart Disease. Grand Central Life & Style (2012).
Kraemer WJ, Volek JS, Clark KL, Gordon SE, Puhl SM, Koziris LP, McBride JM, Triplett- McBride NT, Putukian M, Newton RU, Häkkinen K, Bush JA, Sebastianelli WJ.
Influence of exercise training on physiological and performance changes with weight loss in men. Med Sci Sports Exerc. 1999 Sep;31(9):1320-9.
Schuenke MD, Mikat RP, McBride JM. Effect of an acute period of resistance exercise on excess post-exercise oxygen consumption: implications for body mass management. Eur J Appl Physiol. 2002 Mar;86(5):411-7. Epub 2002 Jan 29.
Tremblay A, Simoneau JA, Bouchard C. Impact of exercise intensity on body fatness and skeletal muscle metabolism. Metabolism. 1994 Jul;43(7):814-8.
van Gent RN, Siem D, van Middelkoop M, et al Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review British Journal of Sports Medicine 2007;41:469-480.